IBM’s Watson Ups the Ante in Healthcare | Sherpas in Blue Shirts
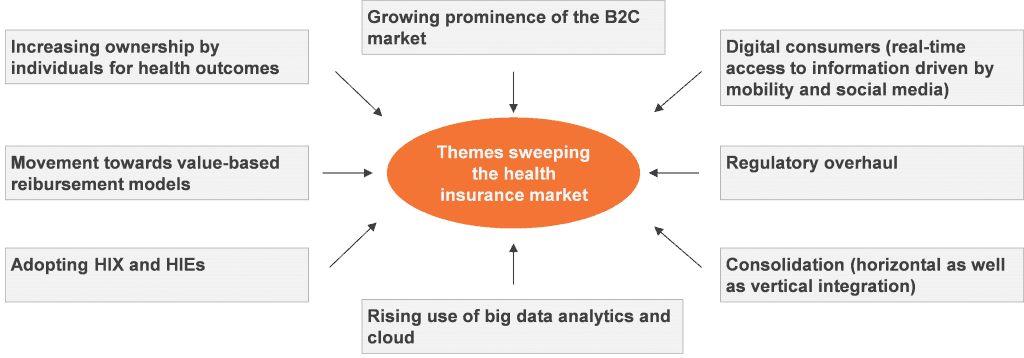
The recently announced acquisition of Merge is one in a string of initiatives by IBM to increase both its market presence and depth of offerings to the healthcare sector. With birth rates increasing in many parts of the world and the aging population growing in developed countries, the race is on for data driven and highly efficient healthcare.
IBM is clearly targeting this market. Its recent activities have included:
- Entering into new partnerships with companies such as Apple, Johnson & Johnson, and Medtronic for health-related data collection, analysis, and feedback
- A partnership with CVS Health to develop care management applications for chronic diseases
- Acquiring Explorys, a healthcare data provider, and Phytel, a hospital care coordination information provider
- Buying AlchemyAPI to include text analysis and computer vision capabilities into Watson’s computing platform
- Establishing a dedicated business unit called IBM Watson Health, headquartered in the Boston, MA, with the specific remit of growing its healthcare business
- Collaborating with leading hospitals and research institutes including Memorial Sloan Kettering Cancer Center, University of Texas MD Anderson Cancer Center, the Cleveland Clinic, and the Mayo Clinic to leverage Watson’s healthcare capabilities at the cutting edge of medical research
- Setting up IBM Watson Health cloud to bring together data for healthcare and research
The US$1 billion acquisition of Merge brings IBM a medical imaging platform to combine with Watson’s image data and analytics capabilities and an extended client base. Excellent and Elementary, Dr. Watson.
With these initiatives, IBM is building specialist competences, to capture, analyze, and recommend treatments or actions that would help healthcare providers, payers, pharmaceuticals, as well as individuals achieve positive health outcomes.
Gaining a wide range of capabilities in specific areas has helped IBM generate specific segment revenue in good and bad times. For example, its large number of information management and WebSphere portfolio acquisitions (e.g., Cognos, Netezza, and SPSS, to name but a few) has seen segment-specific revenues maintain steady growth over the years.
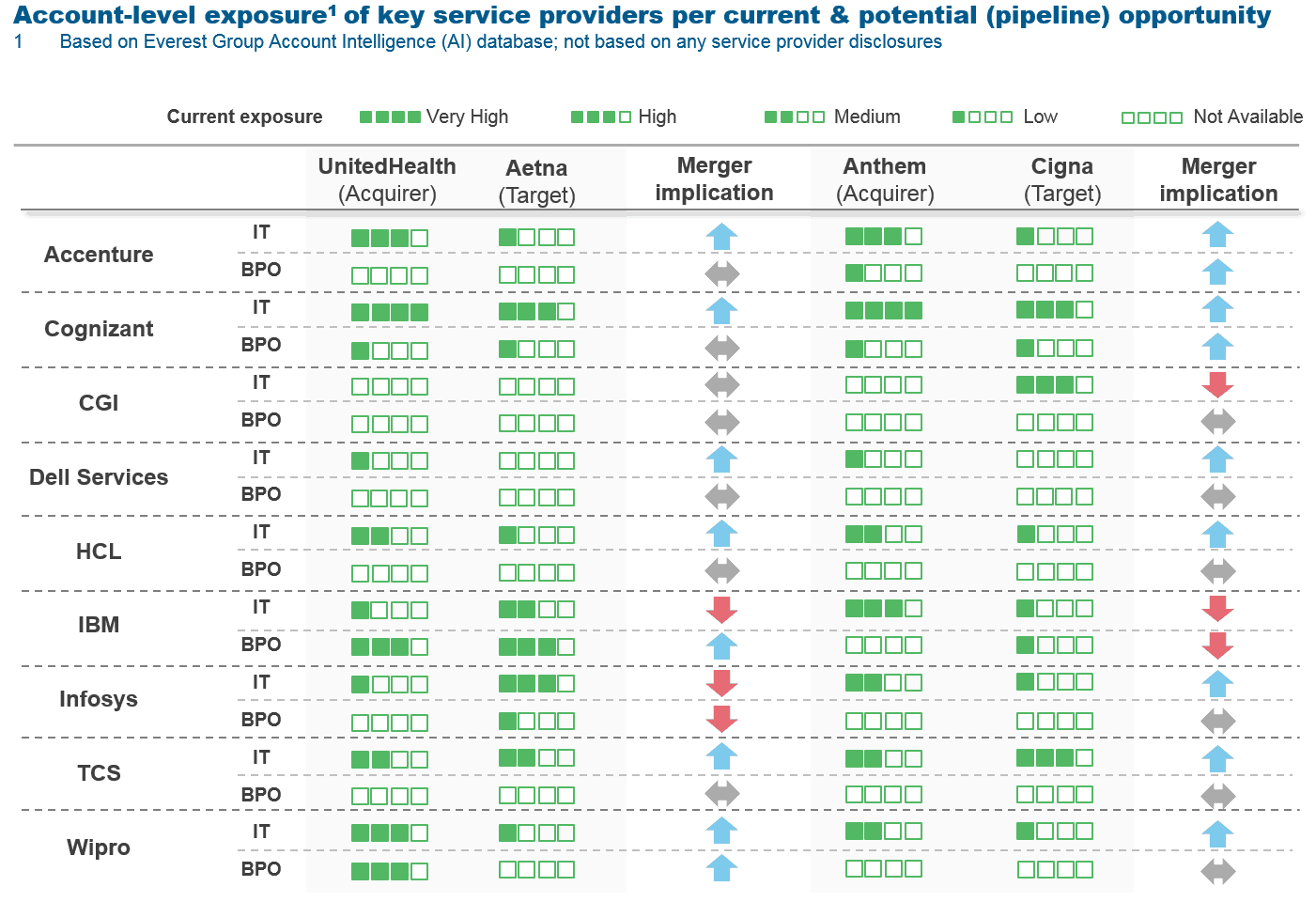
If IBM was to successfully combine its deep specialization in healthcare with Watson’s cognitive computing to enhance its services, it could gain a big edge over competitors at a time when demand is set to grow. At the moment we are seeing more of IBM in healthcare IT infrastructure modernization contracts than data-driven care provisioning and support services. Recent examples include:
- A contract to update the UK NHS’ electronic staff record (ESR) system, adding mobile access and self-service capabilities for 1.4 million employees
- A contract to provide mainframe and data center server and storage infrastructure services for Anthem Inc, a U.S.-based health benefits company, for the next five years at TCV of US$500 million
These types of contracts give IBM opportunities to tap into new solution and services openings at existing clients.
Other challenges for IBM’s intelligent and data driven healthcare offerings include:
- Collecting enough data for its solutions to be relevant to, as well as accessible in, different parts of the world
- Data protection barriers in Europe
- Poor cloud infrastructure in emerging economies.
IBM is going all out when it comes to showcasing Watson as a competitive differentiator. In an uncharacteristic move (and a sign of the times), it has launched Watson Developer Cloud, an open platform for developers to build apps on top of Watson for industry-specific solutions (through a set of APIs and SDKs). It is also working with app developers such as Decibel, Epic, Fluid, Go Moment, MD Buyline, TalkSpace, and Welltok to build apps embedded on Watson technology, thereby, rounding up a robust ecosystem. It is abundantly clear that IBM views healthcare as the principal vertical where Watson’s computing prowess can make its mark. In the meantime other service providers are likely to build or acquire their own cognitive capabilities to challenge IBM on pricing and specialist offerings.
Photo credit: Flickr