Payers are undergoing rapid transformation to meet growing expectations around value-based care, proactive population health management, and quality-linked reimbursement. Care management platforms are emerging as foundational infrastructure, enabling payers to manage chronic conditions, close care gaps, enhance regulatory reporting, and improve member outcomes.
Recent advances have expanded platform capabilities beyond documentation to include AI-powered orchestration, real-time analytics, and interoperability frameworks that integrate Electronic Health Records (EHRs), claims, labs, pharmacy data, Social Determinants of Health (SDoH), and wearables. Providers are embedding generative AI for care plan automation, conversational interfaces, and summarization of clinical records, while agentic AI is beginning to support decision-making in areas such as prior authorization. Despite these innovations, challenges remain in seamless EHR integration, limited workflow automation, and uneven adoption of next-generation capabilities.
As a result, buyers are prioritizing platforms that deliver scalability, automation, user-centric design, and interoperability with other systems. Providers are differentiating through domain-specific capabilities (for example, chronic disease management and behavioral health), stars optimization, and interoperability maturity.
-
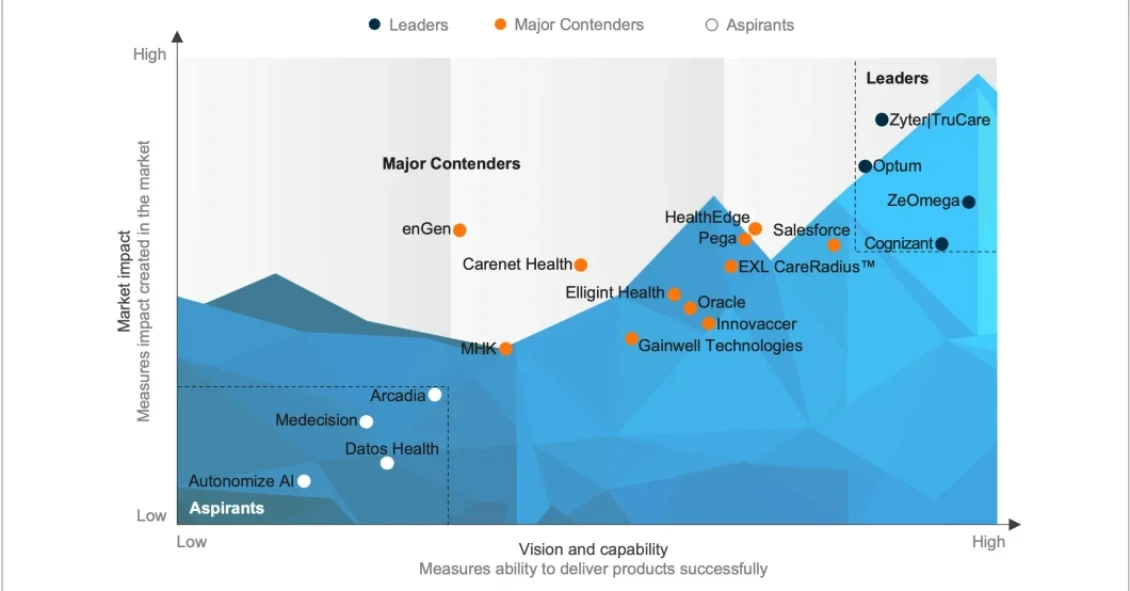
Care Management Platforms for Payers PEAK Matrix® Assessment 2025
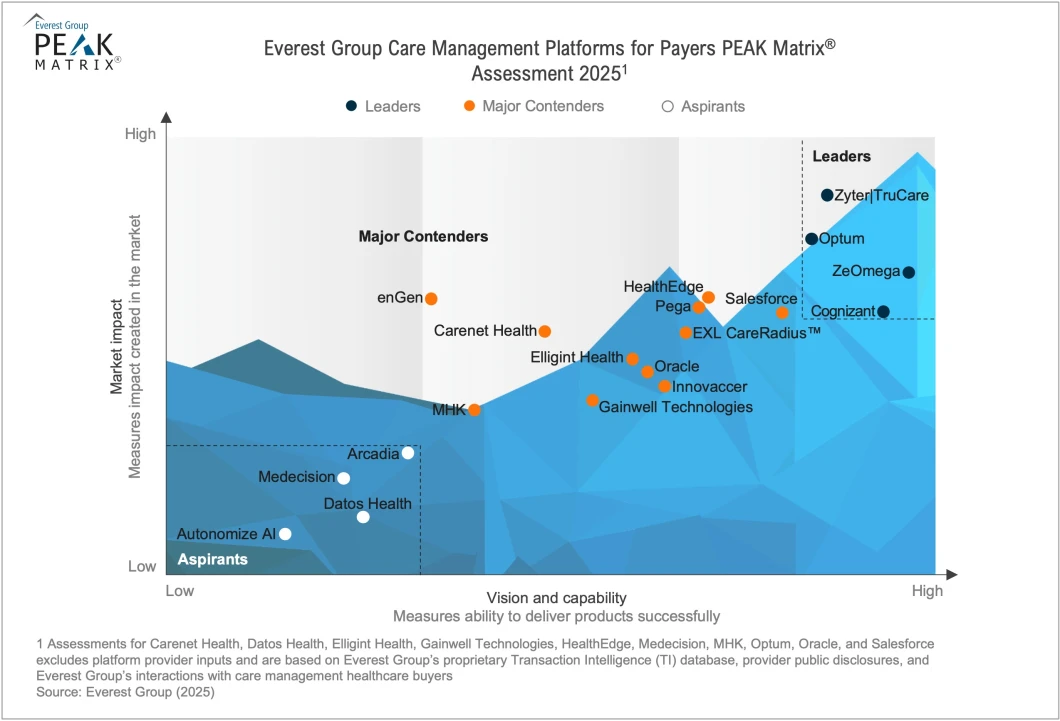
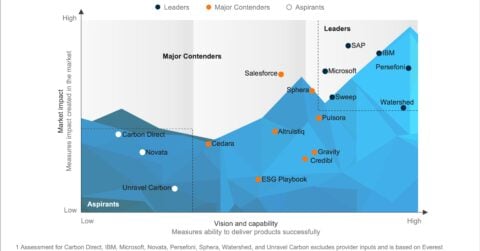
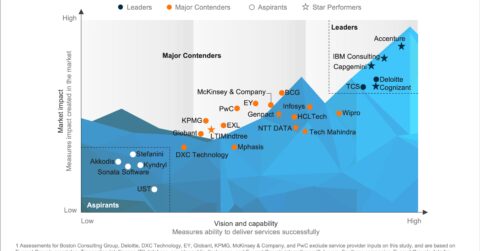
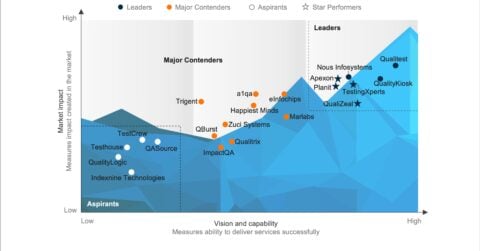
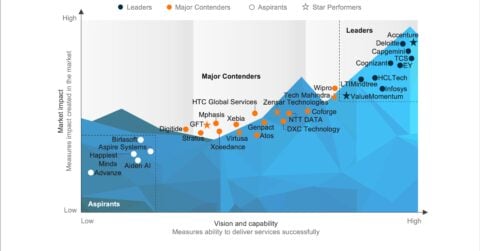
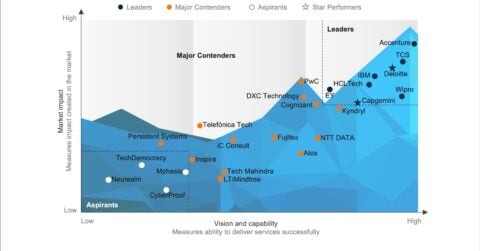
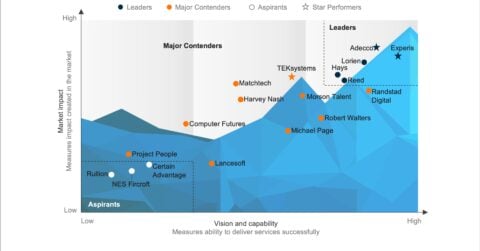
In this report, we assess 19 care management platform providers, positioning them as Leaders, Major Contenders, and Aspirants based on vision, capability, and market impact. The analysis draws on Everest Group’s annual RFI process, provider briefings, buyer interviews, and proprietary market research.
Scope
- Industry: healthcare
- Geography: global
- Domain: care management for payers
Contents
In this report, we:
- Evaluate 19 care management platform providers using Everest Group’s PEAK Matrix® assessment framework
- Examine technology investments across generative AI, agentic AI, and SDoH integration
- Highlight buyer expectations around UX, interoperability, configurability, and data maturity
- Provide strategic sourcing guidance and differentiate providers by functionality, scalability, and domain fit
READ ON
What is the PEAK Matrix®?
The PEAK Matrix® provides an objective, data-driven assessment of service and technology providers based on their overall capability and market impact across different global services markets, classifying them into three categories: Leaders, Major Contenders, and Aspirants.