
On Friday, October 14, the Centers for Medicare & Medicaid Services (CMS) in the United States released a humongous, 2398-page rule to implement new value-based payment programs under the Medicare Access and CHIP Reauthorization Act (MACRA).
This release is a significant step forward in streamlining Medicare payments, and establishing what “value” will mean in the much debated Value-Based Reimbursement (VBR) programs.
Here’s our initial take on this release, in order of what I liked most about the rules.
CMS is making the right noises: As the CMS acting administrator, Andy Slavitt, put it, “…..changes to the rule were to help physicians focus on delivering care and seeing patients instead of performing administrative tasks.” The term in bold represented the point of conflict between a right thinking, efficiency-focused regulator and unnecessarily overburdened physicians.
How is some of this getting addressed?
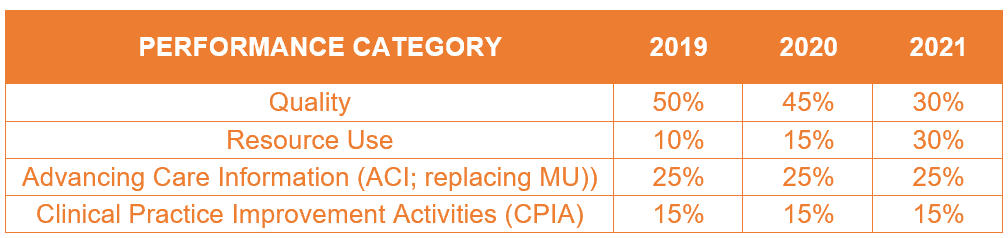
Reduces confusion over quality improvement: The new set of rules consolidates three existing quality reporting programs — Physician Quality Reporting System, Value-based Payment Modifier, and Meaningful Use (MU))– and a new performance category into a single system through Merit-based Incentive Payment System (MIPS.) The definition of “merit” or value was never clearer. Here is a snapshot of the scoring model that defines the four performance categories and their weights:
Pick Your Pace (PYP): In order to make the above operational, CMS is allowing providers to pick their own pace, (see Andy Slavitt’s blog for more details), and choose from three data submission options or join an advanced Alternative Payment Model (APM):
- Test the program
- Submit 90 days of data
- Submit a full year of data
Enabling consortiums: CMS now allows MIPS reporting as a group, enabling smaller providers to get a better deal. What this means is that a group of clinicians sharing a common Tax Identification Number (irrespective of specialty or practice site) can group together to receive payments based on the group’s performance. This will foster necessary consolidation in the ambulatory space.
Relaxes exclusion norms through APMs: Providers not eligible for MIPS can still receive a bonus payment for meeting performance criteria through qualifying APMs. The inclusion criteria are clearer than before, and the nervousness caused by stringent exclusion norms is largely addressed.
Last, but not least, provides a further fillip to IT: While use of certified EHR technology will continue to give providers brownie points for performance, the following five required measures that CMS has mandated for providers will further boost technology adoption:
- Security risk analysis
- E-prescribing
- Provide patient access
- Sending summary of care
- Request/accept summary of care
Net-net, this new rules release is a great move forward toward settling the debate on “value,” and will energize the healthcare industry to spend more on technology. As you wade through the 2398 pages, watch this space for more of our explanations and perspectives on this topic.










