Health plans and payer organizations rely on core administration platforms as the foundation of their operations. These platforms facilitate the efficient execution of core operational and administrative functions such as benefits administration, claims processing, member enrollment, claims payment and adjustments, and product management for benefits and product lines. However, the legacy Core Administrative Processing Solutions (CAPS) are inadequate in keeping up with the rapidly evolving delivery and implementation options and IT systems integration. These systems have been stable and reliable for decades but are often highly customized to the client’s requirements and are hosted on the premises. As a result, there is significant inertia in transitioning from legacy solutions to modern cloud-based core administration solutions due to the associated risks and efforts required.
The healthcare industry is now seeking new vendor partnerships due to the rapidly evolving industry compliance and regulatory requirements, challenges and opportunities for payment reform, and the emergence of value-based care.
-
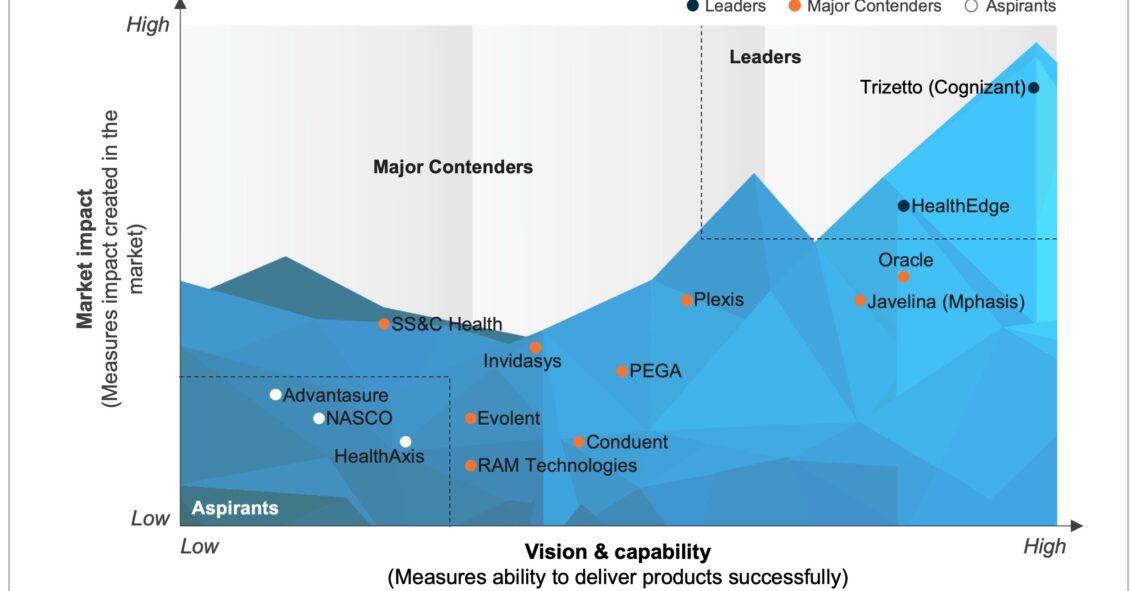
Healthcare Cloud-based Core Administration Platforms PEAK Matrix® Assessment 2023
What is in this PEAK Matrix® Report
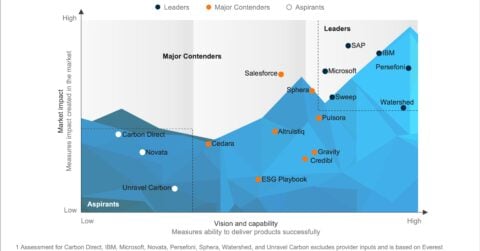
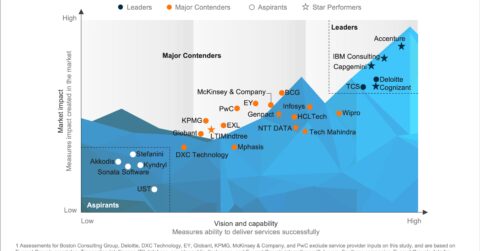
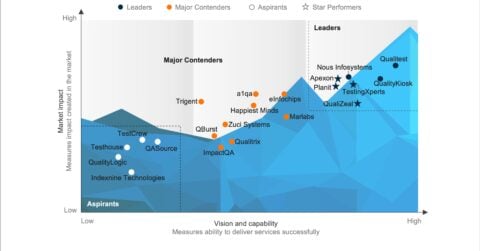
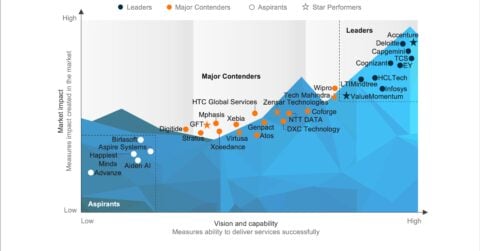
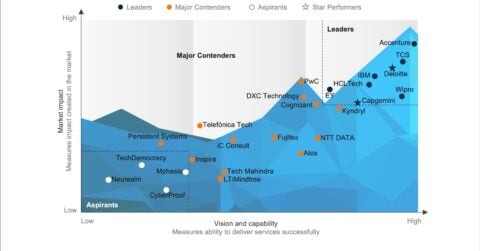
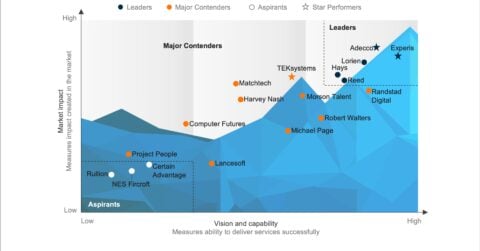
In this report, we assess 14 healthcare core administration platform providers and position them on Everest Group’s PEAK Matrix® as Leaders, Major Contenders, and Aspirants based on their vision and capability and market impact. The report also outlines the strengths and limitations of each provider.
Content:
In this report, we examine:
- 14 healthcare core administration platform providers featured on the Healthcare Cloud-based Core Administration Platforms PEAK Matrix®. The assessment is based on Everest Group’s annual RFI process for the calendar year 2022, interactions with leading healthcare core administrative processing platform providers, client reference checks, and ongoing analysis of the US healthcare CAPS market
- The characteristics of Leaders, Major Contenders and Aspirants and assessment of capabilities of all the platform providers
- In-depth analysis of sourcing considerations for each of the platforms assessed
Scope:
- Industry: healthcare
- Geography: US
- The assessment is based on Everest Group’s annual RFI process for the calendar year 2022, interactions with leading healthcare core administrative processing platform providers, client reference checks, and an ongoing analysis of the US healthcare CAPS market
READ ON
What is the PEAK Matrix®?
The PEAK Matrix® provides an objective, data-driven assessment of service and technology providers based on their overall capability and market impact across different global services markets, classifying them into three categories: Leaders, Major Contenders, and Aspirants.