Blog
Healthcare Interoperability Is Coming – How Your Enterprise Can Navigate the New Rules

With the deadline for the first phase of the healthcare interoperability rule coming July 1, are enterprises fully prepared to accommodate the changes and the interoperability mandate as a whole? Our three-part blog will guide your organization throughthe regulatory implications, implementation approach, and future opportunities. To learn more about the evolution of interoperability and the challenges enterprises face in deciphering the new regulations, read on.
After decades of trying, interoperability is getting closer.
The Interoperability and Patient Access final rule has provided the impetus needed to finally bring together data from healthcare payers, providers, and health information technology (HIT) vendors for patients to easily access information and coordinate their healthcare.
Announced in 2019 by the Centers for Medicare & Medicaid Services (CMS) and The Office of the National Coordinator for Health Information Technology (ONC), the final rule laid down definite protocols and data standards to comply with unified data transmission between members, payers, and providers.
Healthcare enterprises originally had until January 1, 2021 to implement the Interoperability and Patient Access final rule. However, concerns over COVID-19 led CMS to push back the deadline for meeting the requirements, giving them until July 1, 2021 to comply. The regulation has provided a necessary push to healthcare enterprises for building a strong IT foundation to spur smooth data transfer among stakeholders and healthcare organizations.
So, what’s the buzz about? What does healthcare interoperability mean?
Simply put, interoperability is the capability of healthcare systems and applications such as Electronic Health Records (EHRs), Electronic Medical Record (EMRs), and claims data management systems to converse with each other and have an effortless information exchange. The vision is for members and patients to be able to access their healthcare data at their convenience.
Healthcare enterprises have been trying to implement interoperable systems within their infrastructure for decades. But many challenges and restrictions regarding technology immaturity and technical and financial debt have restricted them from achieving full interoperability. This started to change in the early 2000s with technological advances and a legislative push toward interoperability.
What changes are coming for healthcare enterprises and healthcare IT vendors?
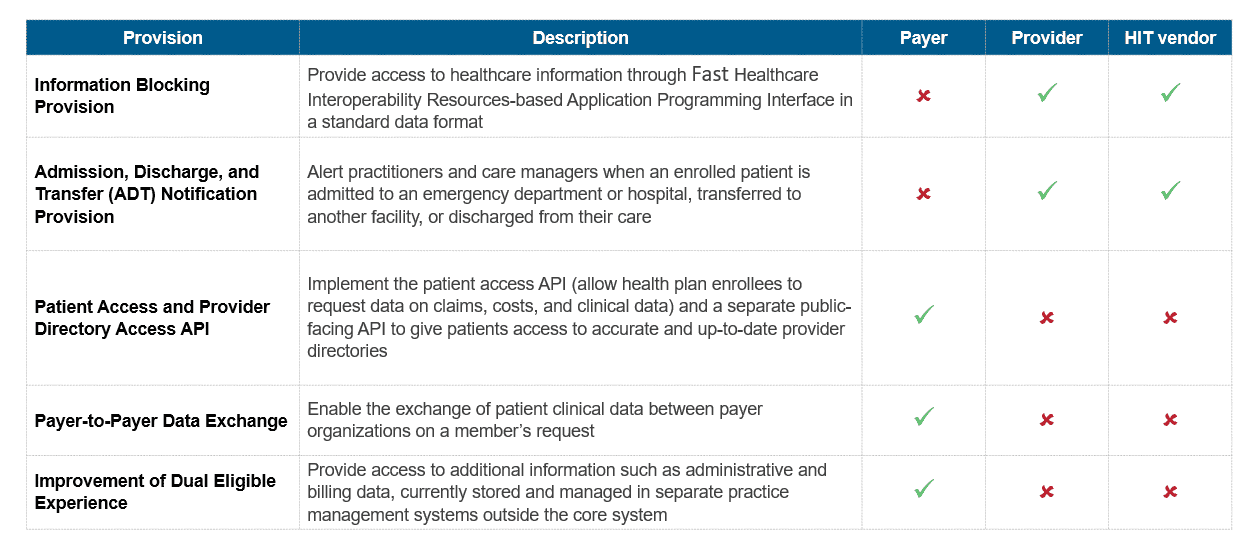
To help healthcare enterprises achieve the goal of making health data accessible to members or patients from anywhere, CMS and ONC have put forward the following key provisions:
What are the biggest challenges healthcare enterprises face to interoperability?
Below are the major hurdles enterprises will need to overcome to implement interoperability:
- Misaligned incentives: The incentives of the stakeholders are misaligned with the goals of interoperability. For example, every HIT vendor currently sells proprietary systems. If interoperability becomes a reality, the customers will no longer encounter proprietary lock-in and will be free to choose any vendor. As a result, interoperability would dilute the competitive advantage of the HIT vendors and cannibalize their existing revenue streams
- Complementary technology enablers: To avoid large upfront investment from each stakeholder, the entire technology framework might be cloud-driven. A host of APIs would need to be developed to enable information sharing between the common platform and the numerous proprietary databases currently used. Similarly, a secure API ecosystem would have to be implemented for external data sharing
- Security of data: Enterprises might require third-party app developers to create their own branded applications for accessing health data. However, there is no regulatory authority over third-party apps and their use of protected health information. Also, with interoperability coming into play, the entire healthcare database might be located at one central platform, making it an easy target for cyber attackers
Interoperability is a journey and an opportunity for healthcare enterprises to assess and remodel their infrastructure. A strong interoperable infrastructure will ensure that healthcare enterprises reap the benefits of their current investments in the long term – enabling them to handle any future technology or industry changes.
To lead the industry, healthcare enterprises need to look beyond the areas defined in the regulation and also focus on a scalable, robust IT architecture, a security-led ecosystem, and the role of analytics in the long run.
To read more about interoperability and emerging opportunity areas in healthcare, read the next installations in our blog series, where we will talk about the interoperability framework and areas of investment for healthcare enterprises. Please feel free to reach out to [email protected] to share your experiences and questions.